WANT TO LEARN MORE?
Reach out for a consultation to learn more about how our clinical programs, software innovations, and revenue enhancements can help you provide quality care and increase revenue
Denials are inevitable. Claims can take years to resolve, and they’re even more challenging if you’re on your own. TMC’s Denial Prevention & Management services are included in our partnerships. We’re committed as your advocate, and we’re ready to get your claims reimbursed.
Learn how our partners are impacted by 5-Claim probes and other CMS denials, and how TMC ensures those claims are paid and the burden of arguing those claims are no longer on the facility.
Our denials team utilizes a hands-on approach in denials, which includes gathering therapy and nursing documentation, writing the appeals and submitting the ADR/denial packets to the requesting party. Our denials team can save you 11 hours per claim by processing your therapy denials.
This effort saves our customers an average of $1,250 on top of their entitled reimbursement.
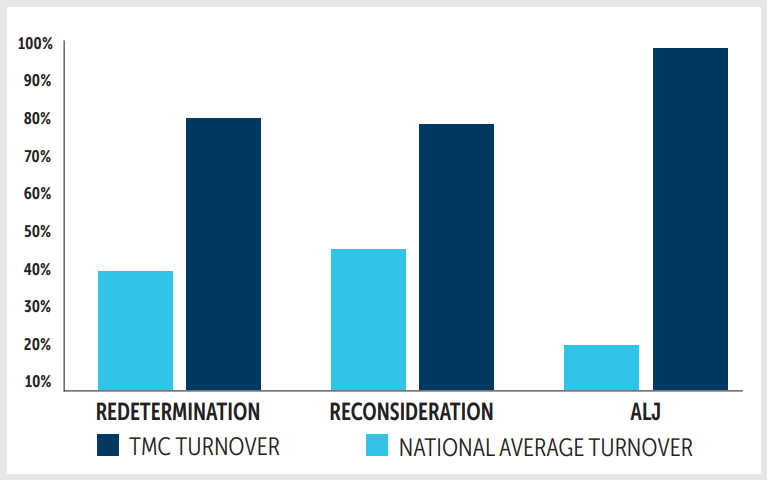
95%. That number represents the success our Denials team boasts in overall denial turnover rate among those using our complete suite of services when compared to customers who try and tackle claims in-house.